Задачи
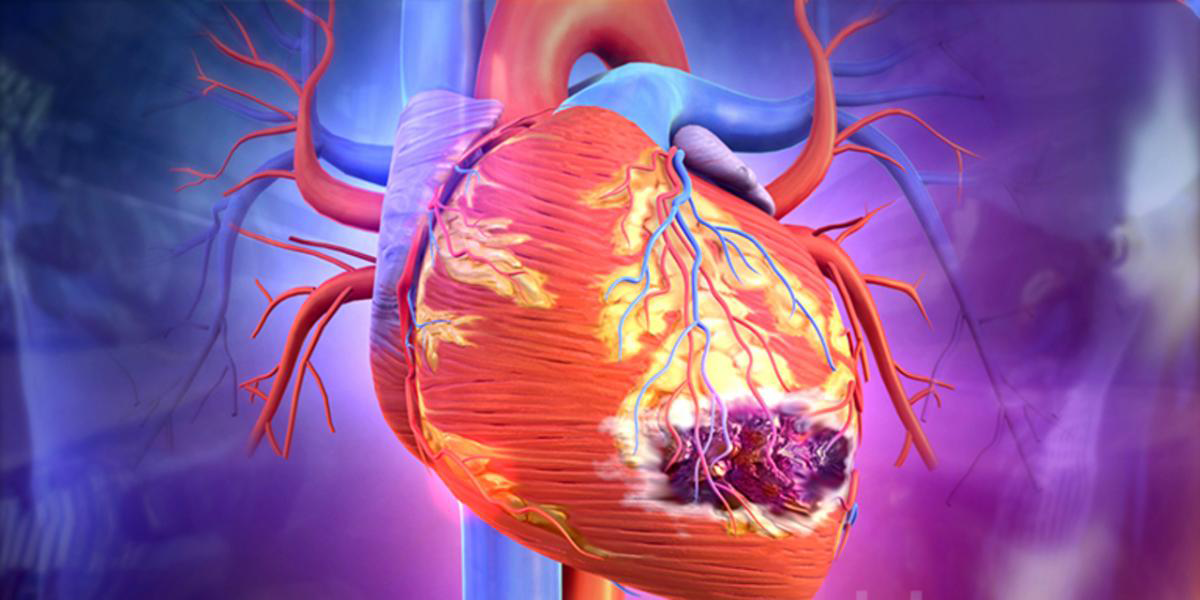 Acute coronary syndrom
Acute coronary syndrom
Study questions
1. What is Acute Coronary Syndrome?
2. What are the Causes of Acute Coronary Syndrome?
3. What are the Signs and Symptoms of Acute Coronary Syndrome?
4. How do you Diagnose Acute Coronary Syndrome?
5. How do you Treat Acute Coronary Syndrome?
6. What is the Prognosis of Acute Coronary Syndrome?
Video 3 Complications of MI15 min
Clinical casesCase 1 The doctor was called home to patient S., 55, who complains of
pressure, burning pain in the chest, radiating to the left arm, under the left
shoulder blade. The attack arose 1 hour ago. Reception of nitroglycerin did not
give effect. The disease is associated with a stressful situation. Objectively: the
general state of moderate severity, clear mind, the body temperature is
36.8 C. The patient is restless, tossing
about. The skin and visible mucous membranes are pale. Breathing rate = 22 per
min. Vesicular breathing. Heart sounds are rhythmic, muffled. Heart rate 96
beats / min., Blood pressure 110/70 mm
RT. Abdominal pathology was not detected. On the ECG, the ST interval is domed
upward displaced, the T wave is fused with an ST interval. Questions 1. Symptoms,
syndromes. Formulate a presumptive
diagnosis. Justify. 2.
Determine management. 3. Additional
methods to study this disease? 4. Create an
algorithm for emergency care in the prehospital phase. 5. Give
recommendations for secondary prevention. Case 2, Patient K., 68 years old, manager. The patient
entered the hospital by the ambulance cardiology team with sharp pain behind
the sternum, arising at night; pain of pressing, burning character, stinging
character, agonizing, disturbing for more than 6 hours. On examination, the condition is grave, sick in
consciousness, but almost does not respond to the environment. Pale gray skin
with cyanotic shade, abundant sticky sweat. Body temperature 37.2 ° C, blood pressure 65/40 mm Hg., pulse 126 in 1
min, rhythmic, weak filling and tension. The borders of the heart are
moderately widened to the left (0.5 cm outwards from the mid-clavicular line);
heart tones are weakened, dull timbre. In the lungs, vesicular breathing is
found in all fields of auscultation; no wheezing. Stomach with palpation is
soft, painless. The liver at the edge of the costal arch, soft, painless. The
spleen is not detectable. Peripheral edema no. 1.
Symptoms,
syndromes 2. Diagnosis, justify. 3.
emergency care. Case number 3. Patient V.,
44 years old, went to the feldsher of the health center with complaints of
compressive pain, located behind the sternum, radiating to the left arm, under
the left shoulder blade, to the left clavicle. Duration of pain 3-5 min. Pain
occures when walking and climbing two floors, they pass away in the rest. This
complaints are noticed about 3 months. Objectively:
the general condition is relatively satisfactory. The skin is a normal color,
the temperature is 36.60 C. Subcutaneous fat is excessively developed.
Vesicular breathing, Pulmonary rate = 20 per min. Heart sounds are rhythmic,
clear. HRate 84 beats / min., Blood pressure 130/80 mm Hg. st. Abdominal
pathology was not detected. 1. Symptoms, syndromes 2.
Diagnostic tests. Diagnosis. 3.Treatment. Case number 4. During the patient's visit to the dentist, he complained of intense
compressive pain behind the sternum continued for about 30 minutes, and
nitroglycerin was ineffective. Previously, pain occurred behind the sternum and
was relieved by nitrates. Three days ago, the pain became longer and repeated
up to 3-6 times a day, relief came only after taking a few nitroglycerin
tablets. During the inspection, the state
- moderate severity. The skin is
wet. Pulse 84 beats per minute, rhythmic. Blood pressure 150/90 mm Hg. Heart
sounds slightly weakened. Another systems - without significant features. 1. Symptoms,
syndromes. Diagnosis 2. Treatment. Case 5 Patient M., 40 years old, was admitted to the clinic 4 hours after the onset of complaints: pain behind the lower part of the sternum of a pressing character and in the epigastric region. An ambulance doctor prescribed aspirin, promedol, 2 doses of nitrospray. At the time of admission, the pain syndrome remained. On examination: BP 110/70 mm Hg. Heart rate 80 per minute. According to the ECG: sinus rhythm, in leads II, III, AVF, a negative T wave was recorded. In the study of troponin, a 10-fold increase in its level was revealed. Questions: symptoms, syndromes. Suggest a diagnosis, write a rationale. Additional investigation. Provide emergency care (if needed). Planned therapy.
Case 6
Patient A., 50 years old, was taken to the hospital unconscious. According to relatives, it became known that about 2 hours ago the patient had an episode of sharp, chest pains, without the effect of taking nitroglycerin.
On examination: serious condition. The skin is pale, moist to the touch, cold, cyanotic. Heart sounds are muffled, rhythmic. Pulse 106 per minute, blood pressure 60/30 mm Hg, the abdomen is soft, painless.
Questions: symptoms, syndromes. Suggest a diagnosis, write a rationale. Additional investigation. Provide emergency care (if needed). Planned therapy.
Case 7
Patient L., a 65-year-old pensioner, turned to dentistry with complaints: pain in the lower jaw. She has had a history of hypertension for ten years. The last two years periodically began to complain of pain in the lower
jaw, which arose when walking accelerated, climbing stairs.
After a short rest, the pain disappeared completely. A month before the present treatment, the pain became more intense and longer (lasted up to 30 minutes), appeared even at rest, during sleep, accompanied by the fear of death.
The dentist who examined the patient diagnosed Ds: pulpitis and removed the tooth. Immediately thereafter, the patient suddenly developed a particularly intense attack of pain in the lower jaw, accompanied by choking, dizziness, cold sweat. Objectively: on examination, the condition is serious. The skin is pale and moist. Pulse of 92 beats per minute, weak filling and tension. BP 80/50 mm Hg Heart sounds are muffled. The number of breaths is 26 per minute. In the lower parts of the lungs, moist rales are heard.
Questions: symptoms, syndromes. Suggest a diagnosis, write a rationale. Additional investigation. Provide emergency care (if needed). Planned therapy.
- 4 февраля 2021, 12:38